One way that nurses formulate their perspective on a disease or condition, and also plan out the way they're going to care for you and intervene therapeutically, is through the use of something called a nursing diagnosis.
A nursing diagnosis, as opposed to a medical diagnosis, looks at something physical or psychological that you may be at risk for, that is within the scope of nursing practice to care for. Consequently, it is a little difficult to find nursing diagnoses related to MRSA specifically, because these diagnoses will be based on the full picture of the patient, and MRSA can present in many different ways.
For example, if you have a wound that is infected with MRSA and refuses to heal, the nursing diagnosis might be:
Impaired skin integrity related to delayed wound healing associated with infection.
After writing this diagnosis, the nurse may create a plan for how to intervene with the situation. In this situation with a wound, their planned interventions may include:
1) Inspect skin in contact with wound drainage for pallor, redness, and breakdown
2) Notify appropriate health care provider (e.g. physician, wound care specialist) if tissue breakdown actually occurs
Their desired outcome may be absence of redness or irritation. They will then evaluate at the end of the shift to see if they accomplished their outcome, which should be measurable.
This particular nursing plan was pulled from this website, which is a very helpful source for nursing diagnoses: http://www1.us.elsevierhealth.com/SIMON/Ulrich/Constructor/diagnoses.cfm?did=427%7C428
Other nursing diagnoses related to MRSA may include (depending on the patient):
Risk for acute/chronic pain
Risk for infection (sepsis) related to release of bacteria into the blood associated with presence of infected necrotic areas
Readiness for enhanced learning
Risk for fluid volume deficit
Nurses learn these nursing diagnoses in school because it trains their mind to think about the whole picture of you as the patient, and not just your medical diagnosis.
Source:
http://www1.us.elsevierhealth.com/SIMON/Ulrich/Constructor/diagnoses.cfm?did=427%7C428
http://www1.us.elsevierhealth.com/SIMON/Ulrich/Constructor/diagnoses.cfm?did=355
MRSAToday
Wednesday, May 20, 2015
Sunday, May 17, 2015
Nursing Care for MRSA
This post will explore the type of care you should receive from a nurse if you are in the hospital (or a clinic) and you have a MRSA infection.
First of all, if you are in the hospital, your room will have a sign outside that says "Contact Precautions". This means that anyone who enters the room (including any visitors) will need to wear a gown and gloves. This is to protect against the spread of MRSA. That is one of the nurse's important tasks.
It is the nurse's responsibility to understand MRSA, and to understand how to properly wear PPE (personal protective equipment) and wash their hands to prevent the spread of infection. Manuals like this one provide nurse's with this information: http://www.health.gov.nl.ca/health/publichealth/cdc/infectioncontrol/mrsa_manual_for_nurses_other_healthcare_workers.pdf.
Another important task of the nurse is to educate you as the patient, so that you understand what MRSA is, how it is treated, and what you can do yourself to get better and to prevent the further spread of MRSA.
Websites like this one will help you learn more about MRSA: http://www.upmc.com/patients-visitors/education/infection-control/Pages/mrsa.aspx.
For example, do you know the difference between MRSA colonization and MRSA infection? MRSA colonization is when the MRSA bug is colonizing on your body (likely in the nares of your nose, or in your armpits for example), but you aren't feeling sick. This can be determined through a nasal swab that is tested in the lab.
A MRSA infection, however, is when the MRSA bug actually invades your tissues. You will start feeling sick (you might have a fever or inflammation), or you might have a wound that won't heal. This is when the infection will need to be treated with antibiotics.
Sources:
http://infectionpreventionuncc.weebly.com/transmission-based-isolation-precautions.html
http://www.health.gov.nl.ca/health/publichealth/cdc/infectioncontrol/mrsa_manual_for_nurses_other_healthcare_workers.pdf
http://www.upmc.com/patients-visitors/education/infection-control/Pages/mrsa.aspx
First of all, if you are in the hospital, your room will have a sign outside that says "Contact Precautions". This means that anyone who enters the room (including any visitors) will need to wear a gown and gloves. This is to protect against the spread of MRSA. That is one of the nurse's important tasks.
It is the nurse's responsibility to understand MRSA, and to understand how to properly wear PPE (personal protective equipment) and wash their hands to prevent the spread of infection. Manuals like this one provide nurse's with this information: http://www.health.gov.nl.ca/health/publichealth/cdc/infectioncontrol/mrsa_manual_for_nurses_other_healthcare_workers.pdf.
Another important task of the nurse is to educate you as the patient, so that you understand what MRSA is, how it is treated, and what you can do yourself to get better and to prevent the further spread of MRSA.
Websites like this one will help you learn more about MRSA: http://www.upmc.com/patients-visitors/education/infection-control/Pages/mrsa.aspx.
For example, do you know the difference between MRSA colonization and MRSA infection? MRSA colonization is when the MRSA bug is colonizing on your body (likely in the nares of your nose, or in your armpits for example), but you aren't feeling sick. This can be determined through a nasal swab that is tested in the lab.
A MRSA infection, however, is when the MRSA bug actually invades your tissues. You will start feeling sick (you might have a fever or inflammation), or you might have a wound that won't heal. This is when the infection will need to be treated with antibiotics.
Besides preventing the spread and providing you with information, the
other nursing care will depend on what sort of infection that you have. If you
have a wound, the nurse will help to clean and dress the wound. The nurse may
also help administer the correct antibiotics ordered for your infection, and
help to treat your fever or other symptoms.
Sources:
http://infectionpreventionuncc.weebly.com/transmission-based-isolation-precautions.html
http://www.health.gov.nl.ca/health/publichealth/cdc/infectioncontrol/mrsa_manual_for_nurses_other_healthcare_workers.pdf
http://www.upmc.com/patients-visitors/education/infection-control/Pages/mrsa.aspx
Saturday, May 9, 2015
MRSA Treatment Recommendations
Clinicians, for example in an out-patient setting, will follow certain guidelines when treating a MRSA skin infection. They will have to follow certain criteria that will dictate the treatment.
If a patient has the signs of a MRSA skin infection, the clinician will first examine whether the skin wound is purulent. The signs of purulence include fluctuance (palpable fluid-filled cavity), yellow or white center, central point or "head', draining pus, and whether it's possible to aspirate pus with syringe or needle.
If the lesion is NOT purulent, the clinician will provide antimicrobial therapy with coverage for Streptococcus, maintain close follow up, and consider adding coverage for MRSA if patient doesn't respond to treatment.
If the lesion IS purulent, the clinician will drain the lesion and send the wound drainage for culture and susceptibility testing. They will educate the patient about wound care and hygiene, and discuss follow-up care with the patient. (For example, if you have a skin lesion it's very important to keep it covered with a dressing, to prevent spreading the infection to others.)
If there are systemic symptoms, severe local symptoms, immunosuppression, or failure to respond to incision and drainage, the physician will consider further antibiotic (oral or IV) treatment focused specifically on MRSA.
The side effects of these treatments depend on the type of antibiotic used. For example, Vancomycin can cause temporary or permanent hearing loss, and also can be toxic to the kidneys.
Interestingly, it was recently found that an Anglo-Saxon potion from 1000 years ago successfully treated the MRSA bug! You can view a video on this phenomenon here:
http://www.cnn.com/2015/03/31/health/anglo-saxon-potion-mrsa/
Source:
http://www.cdc.gov/mrsa/pdf/Flowchart_pstr.pdf
http://www.livestrong.com/article/110099-drugs-used-treat-mrsa/
http://newsroom.ucla.edu/releases/new-guidelines-for-treating-skin-268853
http://www.cnn.com/2015/03/31/health/anglo-saxon-potion-mrsa/
Sunday, May 3, 2015
Signs and Symptoms of MRSA
When trying to identify MRSA through signs and symptoms, one important clue is a wound that refuses to heal, or doesn't respond normally to antibiotics. Please view the video below for a summary:
This video explains how a wound that doesn't want to heal is a huge clue to the presence of a MRSA infection. If a wound is consistently infected (signs of infection include inflammation, irritation and discharge) this could be a sign that you're dealing with a resistant bacteria.
MRSA wounds may appear as a small red bump.
MRSA wounds are often mistaken as a spider bite.
Cellulitis could occur - this is an infection of the skin causing symptoms similar to a sunburn.
MRSA infection can also create an abscess (a lump that's filled with pus).
These are all signs of a skin infection. Signs of a more serious MRSA infection include:
- Bone pain
- Chest pain
- Chills
- Drainage of pus
- Fatigue
- Fever
- Headache
- Joint pain
- Malaise (feeling unwell)
- Muscle aches
- Rash
- Shortness of breath, and painful breathing
If you are experiencing any of these signs or symptoms, especially a wound that will not heal, I recommend seeing your health care provider and being tested for MRSA.
Sources:
https://www.youtube.com/watch?v=1gH8oGH-95E
http://www.webmd.com/skin-problems-and-treatments/ss/slideshow-closer-look-at-mrsa
http://www.healthcommunities.com/mrsa-infection/causes-symptoms.shtml
Sunday, April 26, 2015
Diagnosing MRSA
Today we will discuss how infection with MRSA is diagnosed.
Initially, you may notice some symptoms of staph infection. You may see a little bump on the skin that looks infected - it might be red and swollen with pus. MRSA infections are commonly initially mistaken for a spider bite. You may have a fever as well - this is when it's time to call your health care provider right away.
A MRSA infection could also become quite severe, especially if it spreads to the bloodstream, or other areas like the heart and lungs (this is more common in those who are already hospitalized). Symptoms of this infection include chest pain, cough or shortness of breath, fatigue, fever and chills, general ill feeling, headache, rash, and wounds that don't heal.
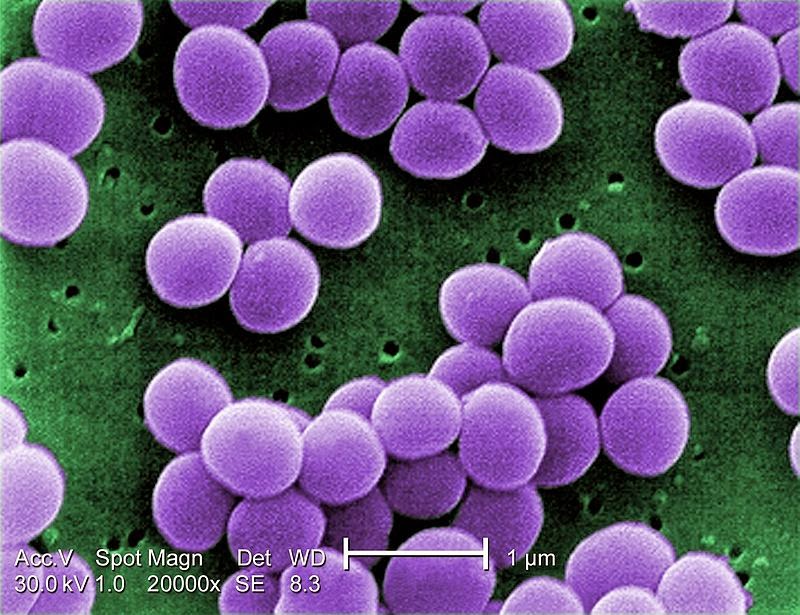
Once infection is suspected, the actual diagnosis is made in the lab. If you have a wound, a health care professional will swab it and take the sample to the lab. The lab will take the sample, place it into a solution, and look for Gram-positive cocci clusters (this describes the color and shape of the stained bacteria).
The sample is tested for Staphylococcus aureus as well. This is done by placing it in a tube with plasma from rabbit's blood and free coagulase. If they find that a clump has formed, this indicates that staph is present.
The next test is to see if this type of bacteria is resistant to medicine. If it continues to grow despite antibiotics, then this is how it is confirmed to be MRSA.
There are also several other ways of obtaining samples to test for MRSA. These include sputum cultures - this is when you simply cough up sputum that can be tested. Urine cultures are also used quite frequently. This could be collected from a foley catheter, or with a cup. If a blood culture is tested and returns positive for MRSA, this would diagnose a bloodstream infection.
Sources:
http://www.cdc.gov/mrsa/pdf/MRSA_Broch_Parent.pdf
http://www.nytimes.com/health/guides/disease/mrsa-infection/overview.html
http://www.wikihow.com/Test-for-MRSA
http://www.healthline.com/health/mrsa#Diagnosis6
Initially, you may notice some symptoms of staph infection. You may see a little bump on the skin that looks infected - it might be red and swollen with pus. MRSA infections are commonly initially mistaken for a spider bite. You may have a fever as well - this is when it's time to call your health care provider right away.
A MRSA infection could also become quite severe, especially if it spreads to the bloodstream, or other areas like the heart and lungs (this is more common in those who are already hospitalized). Symptoms of this infection include chest pain, cough or shortness of breath, fatigue, fever and chills, general ill feeling, headache, rash, and wounds that don't heal.
Once infection is suspected, the actual diagnosis is made in the lab. If you have a wound, a health care professional will swab it and take the sample to the lab. The lab will take the sample, place it into a solution, and look for Gram-positive cocci clusters (this describes the color and shape of the stained bacteria).
The sample is tested for Staphylococcus aureus as well. This is done by placing it in a tube with plasma from rabbit's blood and free coagulase. If they find that a clump has formed, this indicates that staph is present.
The next test is to see if this type of bacteria is resistant to medicine. If it continues to grow despite antibiotics, then this is how it is confirmed to be MRSA.
There are also several other ways of obtaining samples to test for MRSA. These include sputum cultures - this is when you simply cough up sputum that can be tested. Urine cultures are also used quite frequently. This could be collected from a foley catheter, or with a cup. If a blood culture is tested and returns positive for MRSA, this would diagnose a bloodstream infection.
Sources:
http://www.cdc.gov/mrsa/pdf/MRSA_Broch_Parent.pdf
http://www.nytimes.com/health/guides/disease/mrsa-infection/overview.html
http://www.wikihow.com/Test-for-MRSA
http://www.healthline.com/health/mrsa#Diagnosis6
Sunday, April 19, 2015
MRSA Pathophysiology
Today we will be looking into the pathophysiology and etiology of MRSA - essentially, looking at how this bacteria causes infection, and why it is resistant to antibiotics.
As mentioned, MRSA is a bacteria that causes infections. According to ScienceDirect, this bacteria is found in the nose, throat, mucous membranes, and skin. It is often harmless. However, as we've talked about it can sometimes infect humans. This can often happen in crowded areas with shared equipment such as a gym, or a hospital. If a nurse or other healthcare provider touches a MRSA carrier, but then does not wash hands before touching another patient, the second patient could become infected. This bacteria could enter the patient's body through a hair follicle, some kind of break in the skin (such as a wound), or through the respiratory tract (Epidemiology and Pathogenesis of C. difficile and MRSA in the Light of Current NHS Control Policies: A Policy review, ScienceDirect).
According to this article, the antibiotic Methicillin was first introduced in 1959-60. Within a year, methicillin-resistant isolates were being reported.
In order to explain how a bacteria can become resistant to an antibiotic, I highly recommend the following video:
Essentially, mutations in the bacterial DNA can cause the bacteria to gain the ability to change in a way that allows them to become resistant to the powers of the antibiotic. MRSA specifically is resistant to beta-latctin antibiotics like penicillin and methicillin. This can make it more difficult to treat, although the story does not end there!
Sources:
http://www.sciencedirect.com/science/article/pii/S2049080112700122
https://www.youtube.com/watch?v=znnp-Ivj2ek
As mentioned, MRSA is a bacteria that causes infections. According to ScienceDirect, this bacteria is found in the nose, throat, mucous membranes, and skin. It is often harmless. However, as we've talked about it can sometimes infect humans. This can often happen in crowded areas with shared equipment such as a gym, or a hospital. If a nurse or other healthcare provider touches a MRSA carrier, but then does not wash hands before touching another patient, the second patient could become infected. This bacteria could enter the patient's body through a hair follicle, some kind of break in the skin (such as a wound), or through the respiratory tract (Epidemiology and Pathogenesis of C. difficile and MRSA in the Light of Current NHS Control Policies: A Policy review, ScienceDirect).
According to this article, the antibiotic Methicillin was first introduced in 1959-60. Within a year, methicillin-resistant isolates were being reported.
In order to explain how a bacteria can become resistant to an antibiotic, I highly recommend the following video:
Essentially, mutations in the bacterial DNA can cause the bacteria to gain the ability to change in a way that allows them to become resistant to the powers of the antibiotic. MRSA specifically is resistant to beta-latctin antibiotics like penicillin and methicillin. This can make it more difficult to treat, although the story does not end there!
Sources:
http://www.sciencedirect.com/science/article/pii/S2049080112700122
https://www.youtube.com/watch?v=znnp-Ivj2ek
Sunday, April 12, 2015
Epidemiology of MRSA
In the previous post, we learned a little about what MRSA is. In this post we will explore the incidence and prevalence of this bacterial infection in the US.
The Center for Disease Control breaks down MRSA infections as occurring in the community, and in healthcare settings.
When MRSA occurs in the community, it is usually a skin infection. While 1 in every 3 people carry staph in their nose (especially healthcare workers), about two in every 100 person carries MRSA.
Skin infections in the community are most likely to happen to athletes, in daycare/school settings, lockers rooms, etc. According to the CDC, "MRSA infection risk can be increased when a person is in certain actuates or places that involve crowding, skin-to-skin contact, and shared equipment or supplies. This might include athletes, daycare and school students, military personnel in barracks, and people who recently received inpatient medical care."
MRSA can also be acquired in healthcare settings. In the hospital, it can be spread from an infected wound or on the hands of a healthcare provider. It can become a very serious infection, especially if it spreads to the bloodstream.
There is good news though - the CDC has studied MRSA in the healthcare setting closely, and are finding from a variety of sources that the number of MRSA infections are declining. According to the CDC, "Invasive MRSA infections that began in hospitals declined 54% between 2005 and 2011, with 30,800 fewer severe MRSA infections. In addition, the study showed 9,000 fewer deaths in hospital patient in 2011 versus 2005." If you're interested in learning more about this data, you can find links to several studies at this webpage: http://www.cdc.gov/mrsa/healthcare/index.html#q1.
References:
http://www.cdc.gov/mrsa/community/index.html#q1
http://www.cdc.gov/mrsa/healthcare/index.html
http://www.naccho.org/topics/WBS/hai.cfm
http://en.wikipedia.org/wiki/Staphylococcus_aureus#/media/File:Staphylococcus_aureus_VISA_2.jpg
The Center for Disease Control breaks down MRSA infections as occurring in the community, and in healthcare settings.
When MRSA occurs in the community, it is usually a skin infection. While 1 in every 3 people carry staph in their nose (especially healthcare workers), about two in every 100 person carries MRSA.
Skin infections in the community are most likely to happen to athletes, in daycare/school settings, lockers rooms, etc. According to the CDC, "MRSA infection risk can be increased when a person is in certain actuates or places that involve crowding, skin-to-skin contact, and shared equipment or supplies. This might include athletes, daycare and school students, military personnel in barracks, and people who recently received inpatient medical care."
MRSA can also be acquired in healthcare settings. In the hospital, it can be spread from an infected wound or on the hands of a healthcare provider. It can become a very serious infection, especially if it spreads to the bloodstream.
There is good news though - the CDC has studied MRSA in the healthcare setting closely, and are finding from a variety of sources that the number of MRSA infections are declining. According to the CDC, "Invasive MRSA infections that began in hospitals declined 54% between 2005 and 2011, with 30,800 fewer severe MRSA infections. In addition, the study showed 9,000 fewer deaths in hospital patient in 2011 versus 2005." If you're interested in learning more about this data, you can find links to several studies at this webpage: http://www.cdc.gov/mrsa/healthcare/index.html#q1.
References:
http://www.cdc.gov/mrsa/community/index.html#q1
http://www.cdc.gov/mrsa/healthcare/index.html
http://www.naccho.org/topics/WBS/hai.cfm
http://en.wikipedia.org/wiki/Staphylococcus_aureus#/media/File:Staphylococcus_aureus_VISA_2.jpg
Subscribe to:
Posts (Atom)